By Geraldine Ohonba
What is Kawasaki Disease?
Kawasaki Disease (KD), also known as mucocutaneous lymph node syndrome, is a rare but serious inflammatory condition that primarily affects children under the age of five. First described by Japanese pediatrician Dr. Tomisaku Kawasaki in 1967, the disease causes inflammation in the walls of medium-sized arteries throughout the body, particularly the coronary arteries that supply blood to the heart. Although the exact cause remains unknown, experts believe it results from an abnormal immune response to an infection or environmental trigger in genetically predisposed children.
Kawasaki Disease is one of the leading causes of acquired heart disease in children worldwide. If not diagnosed and treated early, it can lead to severe cardiovascular complications such as coronary artery aneurysms, myocarditis, and arrhythmias. Despite its potential severity, most children recover completely if treatment is administered promptly within the first 10 days of illness.
The disease occurs in three phases—acute, subacute, and convalescent—and is characterized by fever, rash, swelling, redness, and inflammation affecting the skin, mouth, and lymph nodes. Although the symptoms often resemble common viral infections, the persistence and combination of features make Kawasaki Disease a unique and potentially life-threatening condition if overlooked.
Causes, Risk Factors, and Pathophysiology
The exact cause of Kawasaki Disease remains a mystery, but ongoing research points to a combination of genetic susceptibility, immune dysfunction, and environmental factors. Scientists suspect that an infectious agent—possibly a virus or bacterium—triggers an exaggerated immune response in some children, leading to widespread inflammation of the blood vessels. However, no single infectious cause has been consistently identified.
1. Genetic Factors:
Kawasaki Disease occurs more frequently in children of Asian descent, particularly Japanese and Korean populations, suggesting a genetic predisposition. Siblings of affected children also have a higher risk, and certain genetic markers, such as variations in the ITPKC and CASP3 genes, have been linked to increased susceptibility.
2. Environmental Triggers:
The disease tends to occur in seasonal clusters, often in winter and spring, indicating possible environmental influences such as airborne pathogens or toxins. Some studies suggest that windborne particles or microbes might play a role in transmitting the unidentified trigger.
3. Immune System Abnormalities:
Kawasaki Disease is considered an immune-mediated vasculitis. The body’s immune system mistakenly attacks its own blood vessels, causing inflammation and damage. This response affects multiple organ systems, including the heart, skin, joints, and mucous membranes.
Pathophysiology:
The hallmark of Kawasaki Disease is vasculitis, or inflammation of blood vessel walls. The inflammatory process causes the arteries to weaken, dilate, and sometimes form aneurysms. The coronary arteries are particularly vulnerable, making cardiac complications the most feared outcome of the disease.
Symptoms, Diagnosis, and Stages
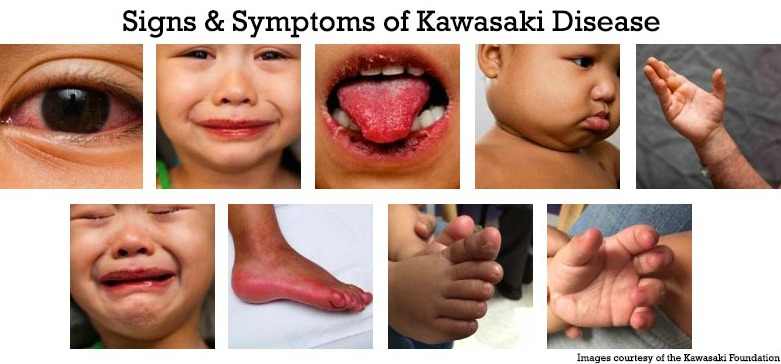
1. Major Symptoms
Kawasaki Disease typically presents with a high fever lasting more than five days, which does not respond well to usual fever medications. Alongside fever, children often develop a combination of the following symptoms:
-
Rash: Usually begins on the trunk and spreads to the limbs.
-
Red eyes (conjunctivitis): Without pus or discharge.
-
Strawberry tongue and red, cracked lips: The tongue appears bright red with visible bumps, resembling a strawberry.
-
Swollen hands and feet: Often red and painful, with skin peeling during recovery.
-
Swollen lymph nodes: Especially in the neck area.
2. Phases of the Disease
-
Acute Phase (Days 1–10): High fever, rash, conjunctivitis, mouth changes, and swollen extremities.
-
Subacute Phase (Days 10–25): Peeling of the skin around fingers and toes, joint pain, and possible heart complications.
-
Convalescent Phase (Days 26–60): Symptoms gradually resolve, but lab tests may still show signs of inflammation until complete recovery.
3. Diagnostic Criteria
There is no specific test for Kawasaki Disease, so diagnosis is based on clinical symptoms and ruling out other conditions. According to the American Heart Association (AHA), a diagnosis is made when a child has a fever for at least five days and at least four of the following five criteria:
-
Rash
-
Swelling or redness of hands and feet
-
Conjunctivitis
-
Mouth and throat changes (e.g., red tongue, cracked lips)
-
Enlarged cervical lymph node (at least 1.5 cm in diameter)
Laboratory findings may show elevated white blood cells, anemia, increased C-reactive protein (CRP), and elevated erythrocyte sedimentation rate (ESR). Echocardiography is often used to check for coronary artery abnormalities.
Treatment, Complications, and Prognosis
1. Treatment Options
Prompt treatment—ideally within the first 10 days of symptom onset—is crucial in preventing serious heart damage. The mainstay of therapy includes:
-
Intravenous Immunoglobulin (IVIG): A high dose of IVIG reduces inflammation and lowers the risk of coronary artery aneurysms when administered early.
-
Aspirin Therapy: Used to reduce fever, inflammation, and blood clot formation. Low-dose aspirin may continue for weeks or months under medical supervision.
-
Corticosteroids: May be added for children who do not respond to IVIG or have high-risk features.
2. Possible Complications
Without treatment, about 20–25% of children may develop coronary artery aneurysms, leading to long-term cardiovascular problems. Other potential complications include myocarditis (inflammation of the heart muscle), pericarditis (inflammation of the heart’s lining), arrhythmias, and heart valve problems. Rarely, the disease can lead to sudden cardiac death.
3. Prognosis and Long-Term Outlook
With timely diagnosis and treatment, most children recover fully and live normal lives without lasting effects. The mortality rate for Kawasaki Disease is less than 0.5% in developed countries. However, children with significant coronary artery damage require lifelong cardiac monitoring and care to prevent complications such as heart attacks later in life.
4. Preventive and Supportive Care
Since the cause remains unknown, there are no specific preventive measures. However, early recognition by parents and healthcare providers is key. Any child with persistent fever and rash should be promptly evaluated by a pediatrician. Emotional and psychological support is also essential, as the disease can be distressing for families.
Kawasaki Disease, though rare, represents a medical emergency in pediatric care due to its potential to damage the heart. Early detection and aggressive treatment are the cornerstones of successful management. With increased awareness, advances in diagnosis, and effective treatment protocols, the prognosis for children with Kawasaki Disease continues to improve significantly. Continued research is crucial to uncover the precise cause and develop targeted therapies that could one day prevent this mysterious illness altogether.

