Depression also known as major depressive disorder is a common and serious mental health condition that negatively affects how you feel, the way you think, and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities you once enjoyed. It can lead to a variety of emotional and physical problems and can decrease the ability to function at work and home. Depression is nearly twice as common in females than in males, according to the Centers for Disease Control and Prevention (CDC).
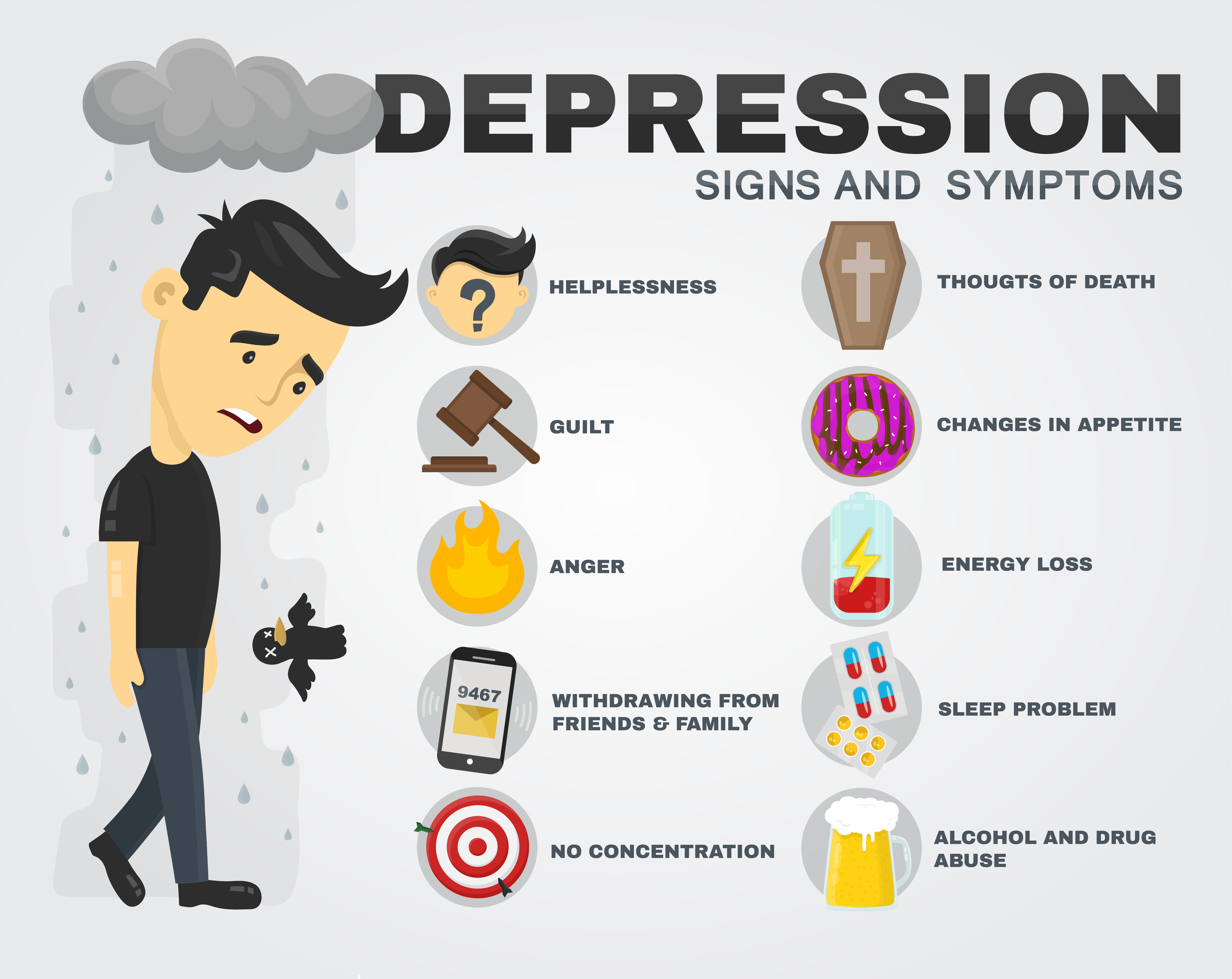
Signs and symptoms
Depression can cause a range of psychological and physical symptoms like persistent depressed mood, loss of interest or pleasure in hobbies and activities, changes in appetite and body weight, unusually slow or agitated movements, decreased energy or fatigue, difficulty sleeping or oversleeping, excessive feelings of guilt or worthlessness, difficulty concentrating or making decisions, thoughts of death or suicide, or suicide attempts
Types of Depression
The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies depressive disorders as the following:
Clinical depression (major depressive disorder): A diagnosis of major depressive disorder means you’ve felt sad, low or worthless most days for at least two weeks while also having other symptoms such as sleep problems, loss of interest in activities or change in appetite. This is the most severe form of depression and one of the most common forms.
Persistent depressive disorder (PDD): Persistent depressive disorder is mild or moderate depression that lasts for at least two years. The symptoms are less severe than major depressive disorder.
Disruptive mood dysregulation disorder (DMDD): DMDD causes chronic, intense irritability and frequent anger outbursts in children. Symptoms usually begin by the age of 10.
Premenstrual dysphoric disorder (PMDD): With PMDD, you have premenstrual syndrome (PMS) symptoms along with mood symptoms, such as extreme irritability, anxiety or depression. These symptoms improve within a few days after your period starts, but they can be severe enough to interfere with your life.
Depressive disorder due to another medical condition: Many medical conditions can create changes in your body that cause depression. Examples include hypothyroidism, heart disease, Parkinson’s disease, and cancer. If you’re able to treat the underlying condition, the depression usually improves as well.
There are also specific forms of major depressive disorder, including:
Seasonal affective disorder (seasonal depression): This is a form of major depressive disorder that typically arises during the fall and winter and goes away during the spring and summer.
Prenatal depression and postpartum depression: Prenatal depression is depression that happens during pregnancy. Postpartum depression is depression that develops within four weeks of delivering a baby. The DSM refers to these as “major depressive disorder (MDD) with peripartum onset.”
Atypical depression: Symptoms of this condition, also known as major depressive disorder with atypical features, vary slightly from “typical” depression. The main difference is a temporary mood improvement in response to positive events (mood reactivity). Other key symptoms include increased appetite and rejection sensitivity.
People with bipolar disorder also experience episodes of depression in addition to manic or hypomanic episodes.
Diagnosis
Screening instruments:
Patient Health Questionnaire-9 (PHQ-9): A 9-item depression scale; each item is scored from 0-3, providing a 0-27 severity score.
Beck Depression Inventory (BDI) or the Beck Depression Inventory-II (BDI-II): 21-question symptom-rating scales providing a 0-63 severity score.
BDI for primary care: A 7-question scale adapted from the BDI.
Zung Self-Rating Depression Scale: A 20-item survey.
Center for Epidemiologic Studies-Depression Scale (CES-D): A 20-item instrument that allows patients to evaluate their feelings, behavior, and outlook from the previous week.
Management
In all patient populations, the combination of medication and psychotherapy generally provides the quickest and most sustained response.
PharmacotherapyAdvertisement
Drugs used for treatment of depression include the following: Selective serotonin reuptake inhibitors (SSRIs), Serotonin/norepinephrine reuptake inhibitors (SNRIs), Atypical antidepressants, Tricyclic antidepressants (TCAs), Monoamine oxidase inhibitors (MAOIs), N-methyl-D-aspartate (NMDA) receptor antagonists & St. John’s wort (Hypericum perforatum).
Psychotherapy
There are a number of evidence-based psychotherapeutic treatments for adults with major depressive disorder. The following have been deemed to have strong research support by Division 12 of the American Psychological Association: Behavior Therapy/Behavioral Activation, Cognitive Therapy, Cognitive Behavioral Analysis System of Psychotherapy, Interpersonal psychotherapy (IPT), Problem-solving therapy (PST), Self-Management/Self-Control Therapy
Evidence-based psychotherapeutic treatments for children and adolescents with major depressive disorder include the following: Interpersonal psychotherapy (IPT), Cognitive-behavioral therapy (CBT), and Behaviour therapy (BT).
Many of these treatments incorporate a parent/family component when working with children or adolescents. In mild cases, psychosocial interventions are often recommended as first-line treatments.
Electroconvulsive therapy
Electroconvulsive therapy (ECT) is a highly effective treatment for depression. The indications for ECT include the following: Need for a rapid antidepressant response, Failure of drug therapies, History of good response to ECT, Patient preference, High risk of suicide, High risk of medical morbidity and mortality, Stimulation techniques, Transcranial magnetic stimulation (TMS) is approved by the FDA for treatment-resistant major depression.
Vagus nerve stimulation (VNS) has been approved by the FDA for use in adult patients who have failed to respond to at least 4 adequate medication and/or ECT treatment regimens. The stimulation device requires surgical implantation.
Complications of depressive disorder
The main complication to highlight is suicide (or attempted suicide):
People who suffer from a depressive disorder have a suicide risk of 30 times more than the general population.
Approximately 15% of patients who suffer from a depressive disorder make at least one suicide attempt.
Complications
Weight gain & Obesity:
MDD can scramble your appetite hormones, so you eat a lot more than normal. Some antidepressants even make you put on pounds. In fact, weight gain is one of the main reasons people stop taking their depression meds.
Chronic Pain:
There’s a strong link between physical pain and depression. They share some of the same neurotransmitters — brain chemicals that act as messengers between nerves. They also share some of the same nerve pathways in your brain and spinal cord. So depression can make you more sensitive to pain, and chronic pain can fuel depression.
Self-Harm:
To manage difficult feelings, you might try to cut or burn your skin, pull out hair, or pick at scabs. Doing drugs or drinking at the same time makes serious injury more likely.
Substance Misuse:
About one-third of people with MDD have a problem with alcohol or drugs. Both can change how your mind and bodywork.
Cognitive Changes:
MDD can change the way your brain works. You might have trouble focusing or remembering a word or someone’s name. This can happen during or between bouts of severe depression. And it can make it harder to function in all areas of your life — work, school, and personal relationships.
Antidepressants may not improve cognitive symptoms, and they might not get better when depression lifts. Other types of treatments may help, though. Cognitive remediation therapy (CRT) teaches you how to overcome brain-related challenges. Common talk therapies, including cognitive behavioural therapy (CBT) and mindfulness therapy, can work well, too.